Navigating Neurodiversity
What is Neurodiversity?
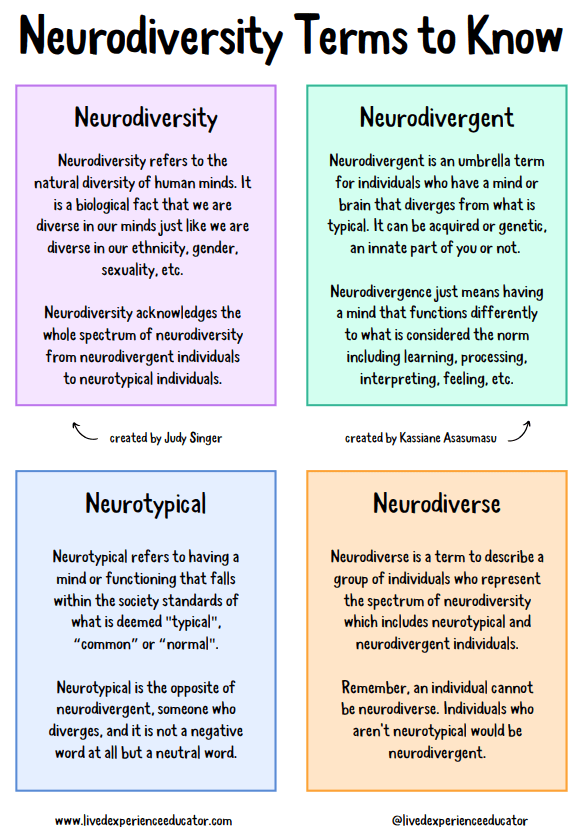
Neurodiversity is a term that refers to the natural differences between people and was coined in the late 1990’s by Australian sociologist Judy Singer. It can be compared to terms such as race, culture, class and gender and is useful to describe people with varying characteristics and behaviours of neurodevelopmental conditions alongside the “neurotypical” majority in a non-prejudiced way. Learning about neurodiversity can help you move the focus from impairments towards everyone’s different abilities.
It is thought that up to 15% of the population are thought to be neurodivergent. The remaining majority are neurotypical.
- 8% of people in the UK are thought to have ADHD.
- 10% of people in the UK are thought to have dyslexia.
- 8% of people in the UK are thought to have dyspraxia.
- 6% of people in the UK are thought to have dyscalculia.
- 1% of people in the UK are thought to have an autistic spectrum condition.
- 1% of people in the UK are thought to have Tourette’s syndrome.
Causes of neurodevelopmental conditions include:
- Genetics
- Trauma at birth
- Infectious disease
- Immune disorders
- Nutritional factors
- Physical trauma
While it is common for neurodevelopmental conditions to occur with co-occurring mental health conditions, (eg. ADHD + bipolar), due to poor awareness it is also common for neurodevelopmental conditions to be misdiagnosed as mental illness. ADHD may also co-occur with physical health conditions, such as Ehlers-Danlos Syndrome (EDS, also sometimes referred to under the umbrella of “hypermobility” although not all EDS patients are hypermobile), Mast Cell Activation Syndrome, and coeliac disease.
Many aspects of society are based on the assumption that there is one form of ‘the human mind’ and accordingly, many systems (education, employment, health and social services, social relationships) have been built up premised on being neurotypical. Building a society that is accessible for neurodiverse people is not only beneficial for everyone, but fair.
‘Neurodiversity may be every bit as crucial for the human race as biodiversity is for life in general. Who can say what form of wiring will prove best at any given moment?’
Robert Blume
Attention deficit hyperactivity disorder (ADHD)
Attention deficit hyperactivity disorder (ADHD) means that the brain has different mental processes to neurotypical people which can affect concentration, activity and impulse levels. People with ADHD can be more likely to experience difficulties with mental health.
There are three subtypes of ADHD
- Inattentive type – this type of ADHD is characterised predominately by inattention and distractibility without hyperactivity.
- Hyperactive/impulsive type – characterised by impulsive and hyperactive behaviours without inattention and distractibility.
- Combined type – the most common type of ADHD, characterised by impulsive and hyperactive behaviours as well as inattention and distractibility.
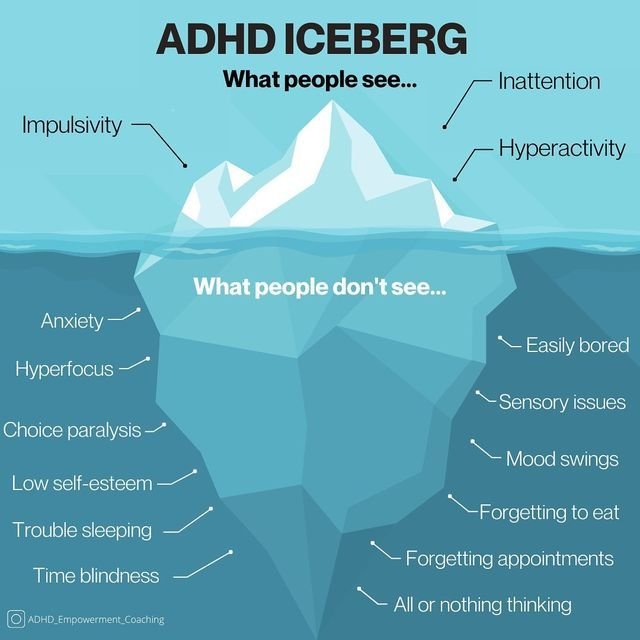
Clients with ADHD may face the following difficulties alongside wider concerns
- Difficulty with attention to detail.
- Often starting new tasks before finishing old ones.
- Difficulty with organisational skills.
- Difficulty focussing or prioritising.
- Often losing or misplacing things.
- Forgetfulness.
- Restlessness.
- Using a direct approach, difficulty in enabling a reciprocal conversation.
- Mood swings, irritability and a short temper.
- Difficulty dealing with stress.
- Feeling impatient.
- Taking risks in activities, which can jeopardise safety.
- Difficulty with executive functioning.
- Rejection sensitivity.
- Difficulty maintaining connection with others.
- Sleep issues.
- Noise and light sensitivity.
- Hyper focus and hyper fixation.
- Low self esteem.
- All or nothing thinking and actions.
- Difficulty adapting to workplace environments and meeting deadlines.
- Time management difficulties.
“There’s often a deep feeling of self-doubt, of not fitting in, of not being accepted or not being good enough. These are based on the negative beliefs attached to difficult experiences and poor interactions that an individual has had, based on how the brain functions with ADHD. They often feel a sense of loss – in experiences that have been missed or damaged, or relationships that have broken down.”
Autism spectrum disorders (ASD)
Autism means that the development of the brain, cognitive style and wider nervous system in autistic people differs from typical neurodevelopment. Clients may benefit from exploring their difficulties or challenges in the following areas alongside wider concerns:
Social Interaction
- Difficulty in recognising and expressing feelings or intentions.
- Difficulty in predicting others.
- Social anxiety that can lead to isolation, breakdown of relationships.
Communication
- Difficulty recognising and responding typically to; tone, intonation, gestures, proximity, facial and body signs.
- Difficulty in gauging when to use types of communication in different settings.
- Difficulty building effective relationships which can cause missed opportunities for achieving rapport and influence.
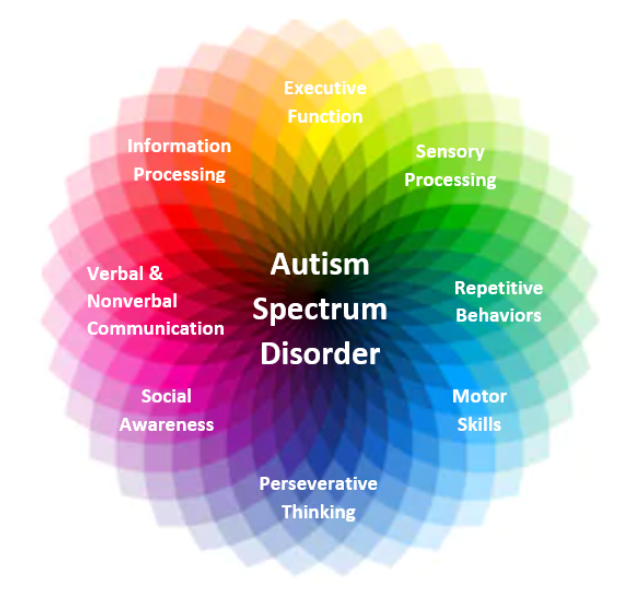
Repetitive and obsessive behaviours
- Behaviours that develop as a therapeutic response to difficulties. They can provide structure, predictability and confidence.
- The impact of society’s perception can affect autistic peoples’ mood, anxiety state, sense of belonging and feeling of acceptance.
Sensory processing
- Sensory processing differences can mean over-sensitivity or under-sensitivity to specific sights, sounds, smells or textures.
- Senses include; touch, auditory, vision, taste, smell, body position (Vestibular) and body sense (Proprioception).
Planning abilities
- Differences in planning ability.
- Difficulty in sustaining attention, shifting between tasks, locating objects and remembering the order of things.
- Difficulty adapting to change and spontaneity.
Camouflaging
- Autistic people may mask their difficulty to fit societal expectations and to feel accepted.
- External behaviour that doesn’t match their internal state can cause emotional and psychological conflict, increasing anxiety and low mood.
Seeking and responding to support
- Difficulty recognising and accessing support which can lead to feelings of isolation and hopelessness.
Obsessions and obsessive compulsive disorder (OCD)
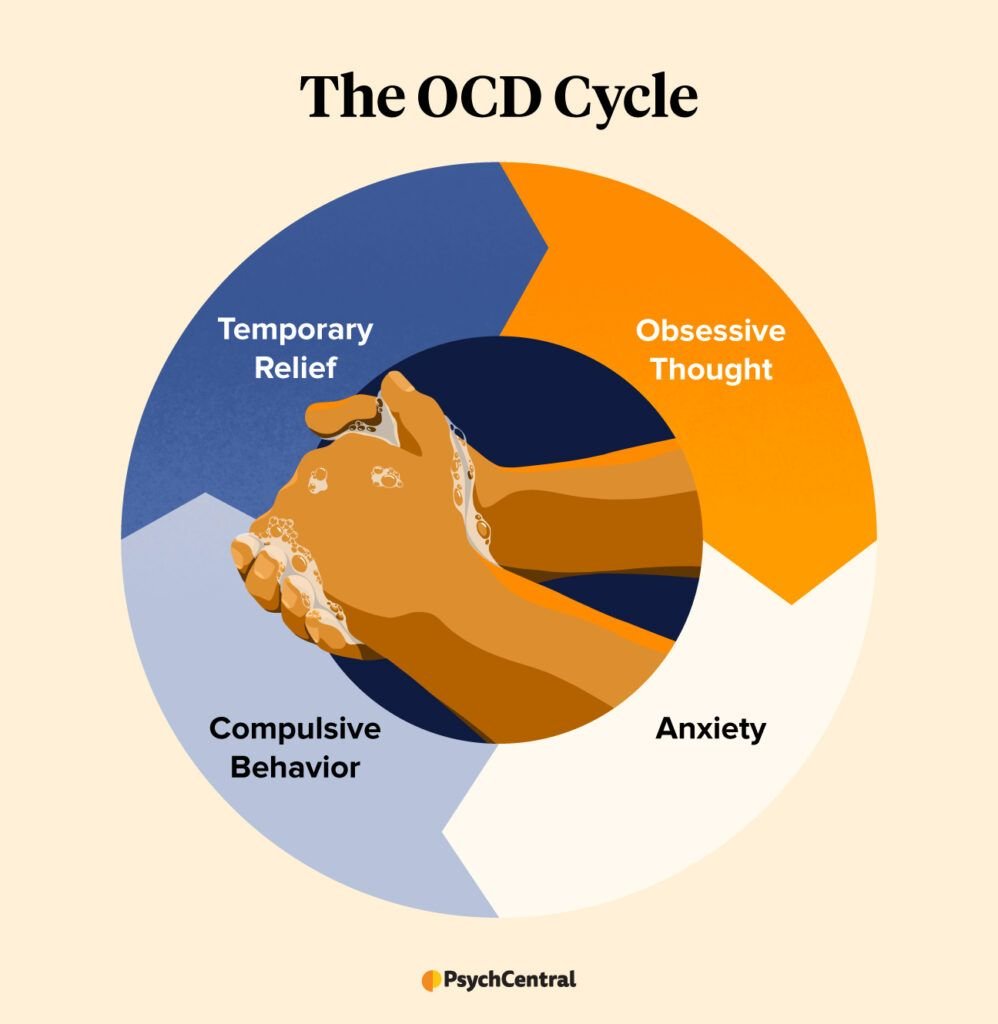
Obsessive-Compulsive Disorder (routinely referred to as OCD) is a serious anxiety-related condition where a person experiences frequent intrusive and unwelcome obsessional thoughts, commonly referred to as obsessions.
Obsessions are very distressing and result in a person carrying out repetitive behaviours or rituals in order to prevent a perceived harm and/or worry that preceding obsessions have focused their attention on. Such behaviours include avoidance of people, places or objects and constant reassurance seeking, sometimes the rituals will be internal mental counting, checking of body parts, or blinking, all of these are compulsions.
Compulsions do bring some relief to the distress caused by the obsessions, but that relief is temporary and reoccurs each time a person’s obsessive thought/fear is triggered. Sometimes over time the compulsions can become more of a habit where the original obsessive fear and worry has been forgotten, in this instance compulsions are often completed to enable the individual to feel ‘just right’, the key word being ‘feel’.
Therapy can help you understand your thought processes and learn how to cope with OCD. It often starts to free you from your compulsions by helping you become less sensitive to them.
“People behave compulsively because they feel discomfort. Therapy is about helping you to understand and work with this discomfort to reduce the physical impact and explore the underlying thought process.”